28 May A Vision for Professionalizing Community Health Workers to Strengthen Health Systems
Reflections from the CORE Group Global Health Practitioner Conference
Since October 2018 when the World Health Organization (WHO) released the WHO Guideline on health policy and system support to optimize community health worker programmes, we at the HRH2030 Program have all welcomed its important recommendations to professionalize community health workers (CHWs). Well-trained and -managed CHWs are essential to harnessing the role of communities in health systems, supporting primary care, and contributing to health outcomes. Earlier this year I helped to disseminate the Guideline through this CORE Group webinar to support implementing the recommendations across diverse contexts.
This month at CORE Group’s Global Health Practitioner Conference (GHPC), I had the privilege of moderating a lively session to further disseminate and reflect on the CHW Guideline. Esteemed discussants included Nazo Kureshy, senior community health advisor at USAID’s Office of Health Systems; Leah McManus, HRH2030’s health workforce informatics technical advisor; Isaiah Ndong, former HRH2030 Senegal country director and currently a Global Health Division director at Chemonics; and Halkeno Tura, director of the Ethnic Minorities of Burma Resource and Advocacy Center (EMBARC).
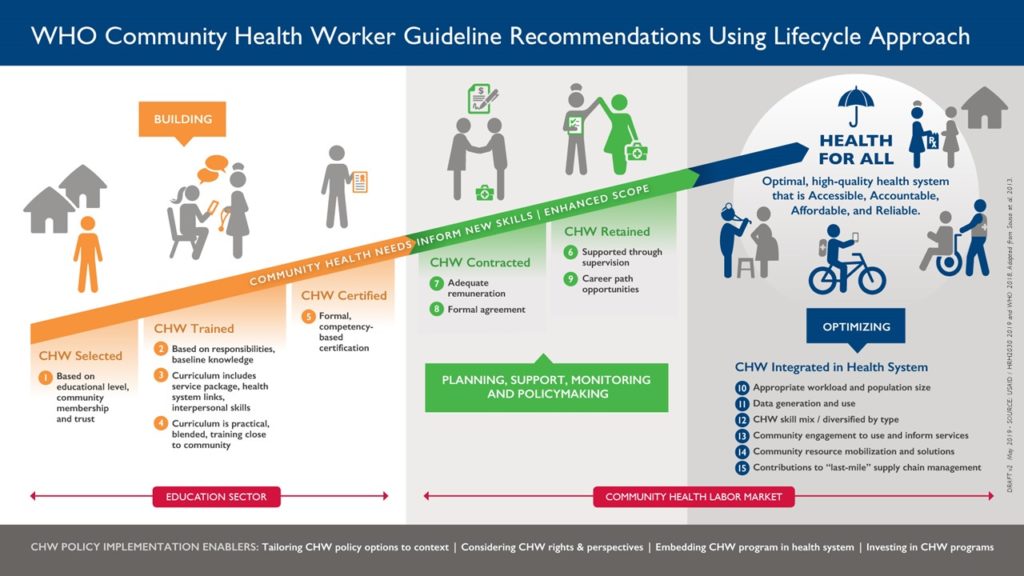
I framed the discussion around a new infographic that we recently created that links the CHW Guideline recommendations to our HRH2030 health worker lifecycle approach. This new CHW adaptation focuses on:
- Building the community health workforce, from selection to training and certification;
- Managing, planning, contracting, supporting and retaining professionalized CHWs;
- Optimizing and integrating CHWs within health systems for greatest impact.
The session’s “fishbowl-style” debate allowed participants to “swim” in and out of the conversation to make their contributions to the key questions discussed:
- Q1: What is the first, and most critical action country leaders should be taking now to implement the @WHO #CHW Guideline recommendations?
- Q2: What is the most important partnership to help ensure we are training the right CHWs in the right health areas?
- Q3: What is the number #1 priority to create a better system to manage and support newly recognized CHWs?
- Q4: What is the most important consideration for optimizing the role of CHWs within health systems to make them more accessible, accountable, affordable, and reliable?
- Q5: What is the most important innovation needed to shape and sustain the role of CHWs in health systems by 2030 and beyond?
.
Answers to the questions above led to an engaged discussion around how CHW programs can help lead to optimal health results. Among my key takeaways were these:
- Defining communities—whether by geography, health issue, culture, and/or language—is important to ground CHW program relevance.
- Health system leaders need to balance investment in CHW programs with broader development initiatives and seek convergences that push countries toward Sustainable Development Goals. For example, recognizing and remunerating unpaid community health volunteers (many of whom are women) can not only improve health outcomes, but also promote decent work, gender equality, and reduce inequities.
- Some core competencies for CHWs should be standardized within programs, with flexibility for others to be responsive to various contexts. An example of a harmonized program shared by a conference participant is the Nigeria Community Health Influencers, Promoters and Services (CHIPS) program.
- Interpersonal skills are important for CHWs to acquire and hone with ongoing supportive supervision to promote quality improvements to care. HRH2030’s forthcoming Enhanced Supervision Landscape Analysis highlights evidence and recommended supervision approaches.
- Without accurate, robust, up-to-date information about the quantity, distribution, skills, and quality of CHWs, decisionmakers will be challenged to effectively plan, finance, and implement CHW programs. The WHO’s National Health Workforce Accounts (NHWA) is an example of a system to monitor health workers, including CHWs, across their lifecycle.
- There remain untapped opportunities to establish viable career paths for CHWs within the health system.
.
We at the HRH2030 Program are continuing to engage in the discussion, especially with the exciting news that just last week, the World Health Assembly #72 acknowledged the value of CHWs to primary health care and universal health coverage by adopting the “CHW resolution” based on the CHW Guideline recommendation.
Do you have ideas to share? Join the conversation on Twitter with the hashtag #OptimizeCHWs.
***
To learn more about HRH2030’s work with community health workers and community health systems, please see:
Untapping the Potential of a ‘New’ Human Resource for Health: the Local Community Leader
The Bostwana Experience with Community-Led Improvement to Achieve HIV Epidemic Control





