11 Dec Reimagining Health Systems for Better Health Requires Better Health Workforce Information
This blog originally appeared on the Frontline Health Workers Coalition website.
It is impossible to reimagine health systems that can achieve better outcomes and social justice goals without a diverse, resilient, well-protected health workforce for all. People drive health system performance—from national ministers of health at the top level to health workers on the front lines seeking to reach the most underserved populations. The problem is that there is an estimated shortfall of 18 million health workers worldwide. And, in too many contexts—whether during crises or when making routine decisions—planners and policymakers do not have a clear picture about how many health workers are actually available and ready to address their communities’ challenges. I gathered many lessons by participating in the Sixth Global Symposium on Health Systems Research (HSR2020). During this conference, I got the chance to discuss ways to reimagine health systems for better health and social justice with members of the global health community.
The Chemonics-led, USAID-funded Human Resources for Health in 2030 Program (HRH2030) envisions a health labor market where all health workers can pursue opportunities and thrive, while improving the health of their communities and nations. To date, HRH2030 has worked in over 30 countries to support governments and their partners to improve health worker performance and productivity, address their competency and skill mix, promote human resources for health management leadership, and increase investments in the health workforce. Much remains to be done to build, manage, and optimize the health and social service workforce to promote decent employment, address gender inequities, support, sustain, and retain the existing workforce, and optimize service delivery to ultimately achieve health for all.
Lessons learned during the recent Ebola outbreak have helped inform what a resilient health system might look like, one with improved health worker data and better informed decision-making capacity. Reimagined, resilient health systems must have five key characteristics:
1. Awareness. High-quality, real-time data is essential. Most policymakers are challenged to understand how many health workers they have, their location, and their current qualifications when making health decisions—COVID-19 has exacerbated these challenges. USAID recommends investing in and promoting access to high-quality data for informed decision-making by strengthening capacities across public, private, faith-based, and community health structures. HRH2030 has collaborated with the World Health Organization and country stakeholders to implement National Health Workforce Accounts in Ethiopia, Indonesia, and the Philippines as a global best practice to improve the quality, availability, and use of health workforce data.
2. Self-regulation. Effective human resources information systems are not built overnight. Most of these systems are the result of health policy mandates, required multisectoral governance, and buy-in from the health, IT, education, labor, finance, and the private sectors. For example, the passing of the Philippines 2019 Universal Health Care Act led HRH2030 to support the creation of a registry of medical and allied health professionals, working with the Department of Health. Engaging the multiple owners of health workforce data helped define and standardize data indicators. As a result, the registry can efficiently compile and integrate health workforce data from many different sources, and data management and use across stakeholders is better coordinated.
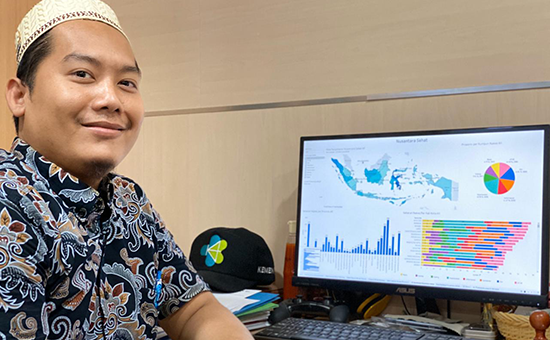
3. Integration. Health worker data is best acted on in conjunction with health information systems and population health data. Applying user-centered digital principles and building informatics competencies across the health system helps develop a skilled workforce that can analyze all available data in support of improving health outcomes. In Indonesia, investments in the health workforce and optimizing information systems—underscored by national policy documents such as the One Data policy and national development plan—proved crucial for supporting health workers during COVID-19. HRH2030 Indonesia rapidly developed and deployed dashboard information on the health workforce in coordination with the Ministry of Health for reference in decision-making during response planning. USAID awarded HRH2030 Indonesia a USAID 2020 Digital Development Award, or “Digi,” for this work.
4. Adaptiveness. Robust, high-quality health worker information systems serve many health systems purposes—from national strategic planning to gender analyses and establishment of communication networks to protect frontline health workers during COVID-19. In Senegal, the national human resource information system is being used to determine immediate gaps and needs during COVID-19. The country’s Ministry of Health and Social Action leveraged the capacity of subnational managers, who were already trained to use the system, applying their knowledge when shifting human resources and performance management functions to a digital platform. In addition, the ministry partnered with telecom company Orange to use its readily available health professional telephone directory to send crucial information on social distancing to frontline health workers via SMS.
5. Diversity. Integrating information about communities’ health into health systems can encourage more stakeholders to access data and take needed action. HRH2030 Mali is using an improved service delivery coverage and responsiveness approach that brings together local health workers, hospital matrons, and community members to review and validate maternal and child health data, resulting in more women and babies getting the essential intrapartum health services that they need. Further, HRH2030 has been developing and using tools to explore facility-community worker models that promote health worker task reallocation and site-level optimization—yet another way to extend more services to more people in an equitable manner.
To achieve reimagined health systems for better health and social justice, let us look for the “triple win” and invest in health worker information systems that can support decent, safe work; strengthen health systems responsiveness and resilience; and deliver better care for more people. By doing so, we will honor the thousands of health workers who have made great sacrifices during this pandemic and show commitment to making the necessary health systems investments to support them.
See HRH2030’s presentation at HSR2020 here.
Photo: Eka Febrianto is an officer in Indonesia’s Human Resources for Health Directorate’s Data and Information Unit, shown here attending a training on business intelligence.





