
26 Nov Getting Health Workers to Where HIV/AIDS Clients Need Them Most with POA
 Liz Pavlovich, MScPH is the Business Development Manager at Touch Foundation, based in the New York HQ office. She works with a mission-driven team across Tanzania, Lesotho, and the US to strengthen healthcare in sub-Saharan Africa, providing better access to care and improving the quality of local health systems. She recently traveled to Mozambique, where Touch Foundation is working with HRH2030 on a health workforce analysis.
Liz Pavlovich, MScPH is the Business Development Manager at Touch Foundation, based in the New York HQ office. She works with a mission-driven team across Tanzania, Lesotho, and the US to strengthen healthcare in sub-Saharan Africa, providing better access to care and improving the quality of local health systems. She recently traveled to Mozambique, where Touch Foundation is working with HRH2030 on a health workforce analysis.
HIV/AIDS services start with the health professional. Yet healthcare workers are often in short supply in sub-Saharan Africa – the region of the world most affected by the epidemic. Another major constraint is the limited amount of funding available. Finally, while some advances have been made in collecting and using data on the health workforce providing HIV/AIDS services, it is often still challenging to get current, reliable data when needed. Yet, this data can power how the global health community most effectively reaches those impacted by HIV/AIDS to ensure that people are tested, and initiated and retained on treatment.
For 15 years, Touch Foundation has developed innovative and data-driven solutions to the training and deployment of the health workforce in Tanzania and elsewhere. Two major health workforce considerations are the skills mix and the geographic distribution. Five years ago, a representative of the Government of Tanzania revealed to us that they had several tens of thousands of requests from districts for new healthcare workers at facilities across the country, but only a fraction of that to deploy, given the low budget available for staffing and modest number of graduates. A solution was needed to make the time-consuming and challenging process of prioritizing these requests easier. With support from USAID and PEPFAR, Touch Foundation created the POA (Prioritization and Optimization Analysis) methodology in 2015 to guide this decision-making process using data on the actual need and real-world budget and healthcare worker shortages.
Recently, we utilized POA, with PEPFAR funding under the USAID HRH2030 Program, to help inform health worker staffing allocations for HIV service delivery in Mozambique. Working with partners, including USAID and CDC, we set out to help stakeholders use data to determine the need and priority of each and every health worker providing HIV/AIDS services at each PEPFAR-supported facility in all provinces of the country. The ultimate goal was to improve the provision of client-centered HIV/AIDS services to achieve epidemic control in Mozambique, a country with one of the world’s highest prevalence rates at 12.6% and lowest health workforce densities.
The POA methodology is simple, yet the results are powerful. Novel to stakeholders involved in health workforce planning, POA begins by assessing the total number of healthcare workers needed to deliver HIV/AIDS services. To do this in Mozambique, we mapped—from a client-centered perspective—the different types of healthcare workers involved in the clients’ care and the amount of time required from each healthcare worker. For example, a clinically stable client on antiretroviral therapy (ART) will be seen by a pharmacist at a health facility for 5 minutes every 3 months in order to collect their ART refills. They are also seen by a clinical officer for 10 minutes twice a year for adherence counseling, monitoring of their health, and lab services. If the number of stable clients on treatment served by that health facility goes up, so too does the need for pharmacists and clinical officers. A clear picture of who is involved in the care continuum for HIV/AIDS clients enabled us to quantify the total number of the various cadres of healthcare workers needed to reach COP 19 targets. Since we also had data on the current health workforce, we could ascertain the health worker shortage by cadre and facility.
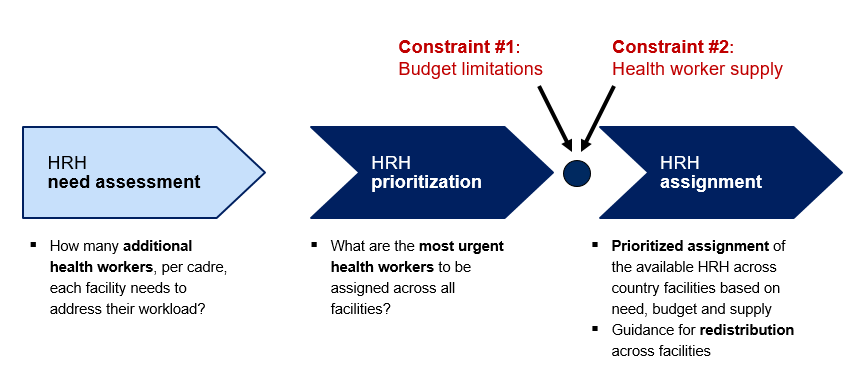
Overview of the POA methodology applied in Mozambique for determining the need for healthcare workers providing HIV/AIDS services, and prioritizing and assigning them based on the budget constraints.
The real innovation of POA is that it prioritizes and recommends assignments for all the needed healthcare workers, taking into the account the limited budgets available to cover their salaries. The needed healthcare workers are ranked so that the top priority assignment is the one that is the most ‘overworked’. For example, imagine a situation where one laboratory technician in a busy facility in Mozambique is struggling to keep up with the viral load testing demands of thousands of clients on treatment, a job for several lab techs. Adding another lab tech at this facility would be much higher priority than a lab tech at a different facility with fewer patients. POA goes through this calculus for tens of thousands of needed healthcare workers to produce a comprehensive ranked list.
While in Mozambique in November, I worked with Touch Foundation staff to orient PEPFAR and CDC stakeholders on how to use the recommendations from POA to decide where to deploy healthcare workers across 595 health facilities. The recommended assignments would cover nearly half of the overall shortage of 18,000 healthcare workers, especially among lay cadres like community and facility counselors. Using POA, implementing partners can more efficiently plan, budget, and staff programs delivering critical HIV/AIDS services.
Through this approach, we improve HIV/AIDS service provision where it’s most needed, by staffing facilities with the optimal quantity and skill mix in order to test, initiate treatment, and retain clients. Data-driven decision-making can bring us closer to controlling the epidemic.
___
Photo: A health worker fills out health records during an immunization event in Mozambique. ©2014 VillageReach, courtesy of Photoshare.





