10 Aug Prioritizing Investments Today to Shape the Health Workforce of the Future
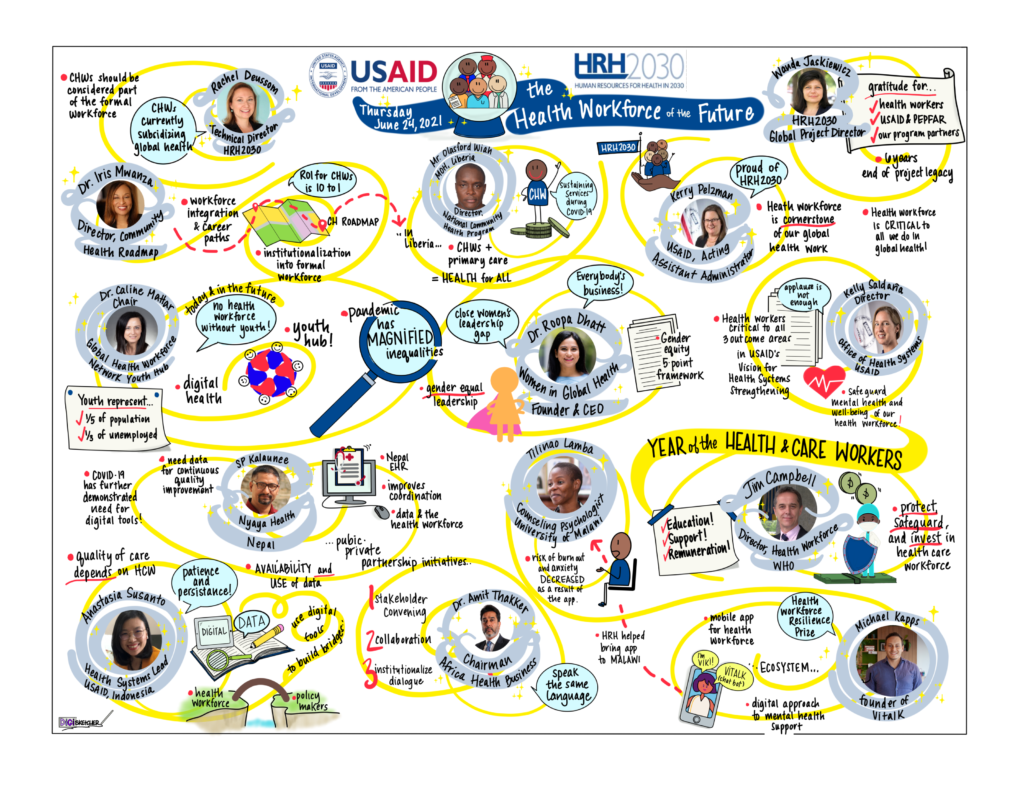
Eight months into the Year of Health and Care Workers, the lessons emerging from COVID-19 are continuing to shape thoughts on the future investments needed for a better protected, supported, and prepared health workforce. Our team at HRH2030 believes that some of the most critical areas that present the biggest opportunities include integrating community health into the overall health system; increasing opportunities for women and youth; driving health workforce decisions with data; and harnessing the power of the private sector – all areas that will also help build a resilient health workforce. We invited several global health practitioners to share their thoughts on this topic at our recent “Health Workforce of the Future” event. Here’s a few highlights.
During her opening remarks, Kerry Pelzman, Acting Assistant Administrator for the Bureau for Global Health, cited the critical investments USAID has made in helping many countries strengthen their health systems, while also noting that, “COVID-19 has further underscored the importance of investment in the health workforce.” She recognized the toll the pandemic has taken on health workers’ well-being, and the discrimination and violence many have faced due to misinformation and stigma related to COVID-19. Despite these challenges, she said, it is encouraging that innovative ideas have emerged to respond to the needs of the future health workforce.
Health Worker Resilience and Mental Health
Art by DigiSketcher Tobey Busch
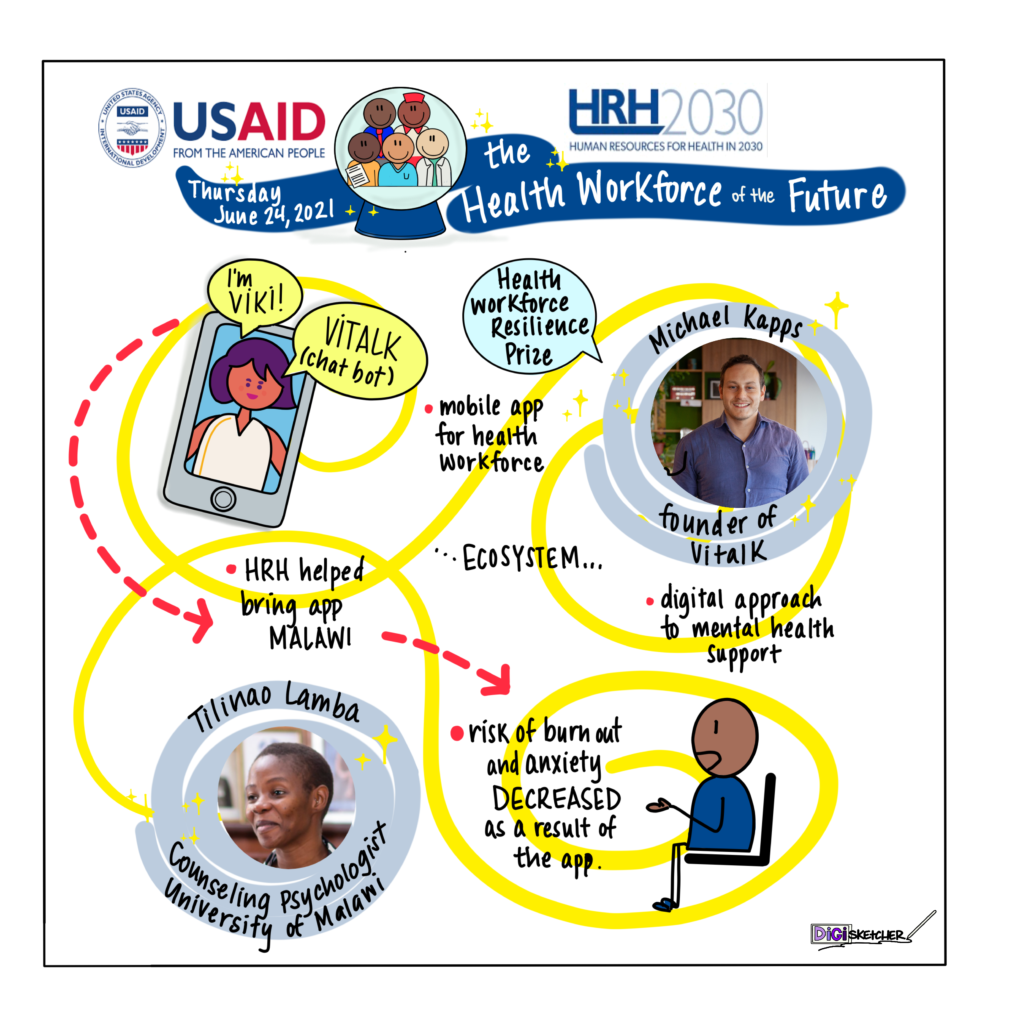
Resilience was a theme repeated throughout the discussion, and we were delighted to have HRH2030 Health Workforce Resilience Prize Winner Michael Kapps with us. Kapps is the founder of Vitalk, an app designed for health workers that uses an artificial intelligence (AI)-powered virtual mental health care assistant for health workers. The app is using technology to break through the stigma of mental health issues, providing techniques and interventions found in traditional therapy via a digital platform that can be used privately at any time. During this last year, with COVID-19 putting a great strain on health workers, the app has shown great promise.
“We’ve reached a milestone of 10,000 healthcare workers using the app in Brazil, where a year ago it was practically zero,” said Kapps. “We’ve also run some studies and are seeing preliminary results that show that just using the app for a number of weeks has a significant effect on reducing some symptoms of anxiety and stress, and in boosting the resilience of the health care workers.”
After receiving the HRH2030 Health Workforce Resilience Prize last year, Vitalk has been working with HRH2030 to adapt and pilot the app in Malawi to see if it could help to address health worker resilience there. Counseling psychologist Tilinao Lamba from the University of Malawi, who is working with HRH2030, noted that mental health isn’t a topic that is much discussed in Malawi, which has few mental health specialists. Health workers are often perceived to be strong, emotionally balanced, and able to take care of others without needing care in return, Lamba says. Despite these perceptions, Lamba found hundreds of health workers who were interested in trying the app. Over a one-month period, health workers using the app reported a lower risk for burnout and decreased risk of anxiety. Based on these results and conversations with many of these health workers, she believes that scaling up the app could make a difference for health workers in Malawi and in other countries, especially those with limited resources and few mental health specialists.
Integrating Community Health into Health Systems
In countries with limited resources where community health workers continue to fill the gaps in the health workforce, the roles they play continue to be unrecognized and undervalued. Investments in community health workers would help fill the health worker shortage and help shape a more diverse workforce that is able to respond to local needs, said Dr. Iris Mwanza, director of the Community Health Roadmap. She underscored that the community workforce should be treated just the same as any other part of the health workforce, stating, “Community health workers should be recognized as an official part of the health system. They should be paid a decent wage; they should be safe doing their jobs; they should have job security, freedom to speak and to organize; and they should have the opportunities and prospects for career development that we all want.” [Learn more about how USAID supports strengthening CHW programs here.]
Equitable opportunities for women and youth
Most of the global community health workforce is women—and women make up more than 70 percent of the health workforce overall. Dr. Roopa Dhatt, founder and chief executive officer of Women in Global Health, noted that despite these figures women health workers fill only a small percentage of leadership roles in the health sector, and they are too often left out of the decision-making process. Many of the policies and interventions related to the pandemic have often been “gender blind and gender harmful” and Dr. Dhatt says it’s time to invest in a “safe, decent, and gender equal workforce for all women in the health and care workforce.” While countries have made commitments to protecting, investing, and safeguarding women before, the pandemic marks a critical time for us to “turn commitments into action,” she said, starting with policy action to build a foundation for equality.
Policies and investments need to be put in place for young health workers, too, said Dr. Caline Mattar. As head of the Global Health Workforce Network Youth Hub, Dr. Mattar sees their contributions to the health workforce clearly. Too often, she says, the global community thinks of youth as either the recipients of health services or the next generation of health workers. They are more than that, she said, noting, “Youth are the workforce of today, as well,” and that they face many of the same challenges as seasoned professionals. Young doctors, nurses, and other health professionals have been integral to the COVID-19 response, she pointed out. They are also helping to change the composition of the workforce, contributing to its diversity, and their approach is more collaborative, especially in the area of digital health. She believes countries and donors should learn from how young health workers are spurring innovation and prioritize investments in creating jobs for young people in the health and care sector.
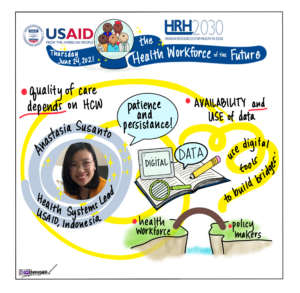
Driving health workforce decisions with data and digital systems
Art by DigiSketcher Tobey Busch
Collaboration is also key to expanding the accessibility and availability of quality data, especially data on the health workforce. USAID Indonesia’s Health Systems Strengthening Team Lead Anastasia Susanto shared how Indonesia has been able to make tremendous strides in ensuring that they have health workforce data to make evidence-informed decisions. Ensuring that data from multiple sources and systems is integrated into the national human resource information system helps to determine where communities have access to health services and where they are lacking. She cited efforts to properly account for midwives in Indonesia, many of whom work in the private sector. “Through HRH2030, USAID facilitated the first-ever MOU between the Ministry of Health and a professional organization, Indonesia’s Midwives Association. This data agreement led to a discussion around health worker careers and accessibility of services,” she said. [Learn more about how streamlining data is supporting Indonesia’s COVID-19 response.]

Art by DigiSketcher Tobey Busch
Elsewhere in Asia, Nyaya Health Nepal is making it easier for hospital staff to do their jobs through a digital health platform, Nepal EHR. An integrated electronic health records system, NepalEHR brings data on patient registration, clinical diagnoses, prescriptions, and supply chain management into one system. It facilitates care across facility and community points of service and allows for continuous improvement in service delivery. SP Kalaunee, former executive director and now a board member, explained that NepalEHR is also integrated into national data systems, ensuring more coordinated care, which has particularly been helpful during COVID-19. By providing so much through one system, NepalEHR enables health workers to do their jobs with greater efficiency and gives them more bandwidth to respond to the changing dynamics that they encounter in their work. As a winner of the HRH2030 Health Workforce Resilience Prize, Nyaya Health Nepal has been able to scale up the system to a total of six hospitals in Nepal, and believes other countries could easily replicate this platform in their own health systems.
Harnessing the Power of the Private Sector
NepalEHR was developed with private sector support, and the development of sustainable health systems can be accelerated through stronger collaboration and partnerships between private and public entities, said HRH2030 Global Project Director Wanda Jaskiewicz. She asked Dr. Amit Thakker, executive chair of Africa Health Business, how his organization has been successful in making that happen. The private sector isn’t one cohesive entity, he noted, saying that it is “fragmented” and efforts to make it more cohesive is one step in activating more partnerships. His organization has been able to bring 27 countries into one federation which is helpful in advancing an overall public-private partnership agenda.
All of these investment areas reflect a whole of society approach to optimizing the health workforce and achieving greater health systems resiliency. In closing the event, and echoing the words spoken by Dr. Roopa Dhatt earlier in the program, Wanda Jaskiewicz appealed to the audience for great collaboration, saying, “Let’s work together to turn words into actions for the future of the health workforce.”
***
The Future of the Health Workforce was the final event in the HRH2030 Program’s End-of-Program Legacy Series. Watch the full event recording here. Below is a visual sketch of the event, captured by graphic artist DigiSketcher, Tobey Busch. Click on the image to enlarge:
Photo caption, from left to right: Wanda Jaskiewicz, HRH2030, Chemonics; Kerry Pelzman, USAID’s Bureau of Global Health; Kelly Saldaña, USAID’s Office of Health Systems; Dr. Jim Campbell, World Health Organization; Michael Kapps, Vitalk; Rachel Deussom, HRH2030, Chemonics; Dr. Iris Mwanza, Community Health Roadmap; Dr. Caline Mattar, Global Health Workforce Network Youth Hub; Dr. Roopa Dhatt, Women in Global Health; Anastasia Susanto, USAID Indonesia; SP Kalaunee, Nyaya Health Nepal; Dr. Amit Thakker, Africa Health Business.